How the Affordable Care Act affects you
What is the Affordable Care Act?
The Affordable Care Act (ACA), also known as the Patient Protection and Affordable Care Act, was passed into law on March 23, 2010. The ACA has many components to it, one of which is the marketplace or exchanges where consumers may shop for their healthcare plans. The marketplace opened for business October 1, 2013, selling medical and dental plans to small employers and individuals with effective dates beginning January 1, 2014.
For more information on the Oregon marketplace, CoverOregon, please visit www.coveroregon.com.
What are essential pediatric benefits?
ACA also has essential health benefit requirements that include essential pediatric benefits. Starting January 2014, most individual and small group insurance plans will have pediatric dental benefits. This coverage may be through a pediatric only plan and/or through a more traditional dental plan that covers the whole family. Large plans could also have this pediatric dental benefit in some cases.
The result of the essential pediatric benefits is that families may have children under 19 with different benefits than the adults, or situations where only the children have benefits. It could even happen that the adults and children have different insurance carriers.
From a plan design standpoint, essential pediatric benefits require that preventive care is covered with no out of pocket for in-network services and that essential services are covered without an annual limit for in-network services. In addition, there are certain benchmark standards for essential pediatric benefits that could result in differences in benefit between adults and children.
In some cases, dental may be offered through a dental plan “embedded” in a medical plan. Embedded means there is only one policy that includes medical and dental coverage. Because there is one policy, the deductible is shared, as well as the out-of-pocket maximum. ODS will be offering plans with embedded dental, but you will still send in your claims with the same process as you would for any other dental coverage through ODS.
What will ODS/Moda Health offer in the new marketplace?
We are selling both individual and group policies through the new marketplace, and directly like we currently do. Consumers eligible for a tax credit/subsidy must purchase through the marketplace to get their credits. As part of preparation for ACA, all existing plans for small groups and individuals are being discontinued and members will roll to a new plan. They will also have the option to pick a different plan. Because of the emphasis on cost, individuals and small groups will be focused on the Preferred Provider Option (PPO) and Exclusive Provider Option (EPO) plans.
A PPO plan means ODS members may choose any network provider (Premier or PPO) to receive their dental care; however, they maximize their benefits when they receive care from a PPO provider.
An EPO plan means that the member must receive care from a PPO provider to receive any benefits. If the dentist is Premier only or non-participating, no benefits are paid.
How will this affect Medicaid?
ACA will be expanding the number of people who are eligible for Medicaid (OHP). This means additional low-income children will receive these benefits. In addition, ODS OHP Standard plan members will roll to the ODS OHP Plus plan in January 2014.
What does this all mean to me, the dental office?
This means that beginning January 1, 2014 your office may begin to see more of your previously non-insured patients now having health coverage. The good news is that there may be more children with dental benefits. This means more potential business for many dentists, especially those who treat children, as well as dentists who are a participating PPO and OHP/Medicaid provider.
For questions about how to become a PPO or OHP/Medicaid provider, please contact our Dental Professional Relations department at 503-265-5720 or toll-free at 888-374-8905.
Also, to learn more about the Affordable Care Act, please visit our Learning Center at https://www.modahealth.com/shop/learning-center.
Examples of ODS Plans
Premier Plans
Delta Dental Premier is the plan that allows patients to choose from the widest possible list of network dentists. The dentist is reimbursed at his/her accepted filed fee.
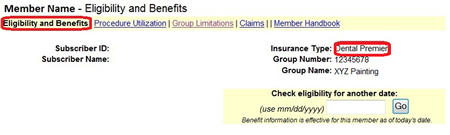
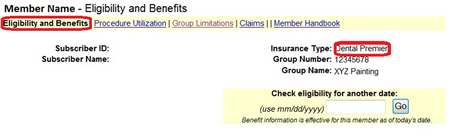
- To identify a Premier Plan on Benefit Tracker:
Insurance type will specify Dental Premier - Group Names and Group Numbers will vary depending on the Employer Group.
Preferred Provider Option (PPO)
The Delta Dental PPO plan utilizes a select group of dentists who have contracted with us at the preferred rate. This plan offers reduced costs for patients who see a preferred dentist. Patients covered by the PPO plan who see a dentist not in the PPO network typically have higher co-payment amounts. The plan provides employers with a lower cost option by utilizing a specific fee schedule with PPO dentists.
- To identify a PPO plan on Benefit Tracker:
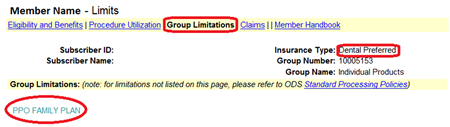
Insurance type will specify PPO (Dental Preferred) plus Group Limitations will show PPO Family Plan.
Family plan is part of the plan name and doesn't mean the whole family is covered. - These plans can be purchased by individuals/families, small groups and large groups so group numbers and group names may vary. Below is an example of a PPO Family Plan, benefit percentages will vary by plan.
- Since both the PPO and EPO plans access the Delta Dental PPO network as the in-network plan, please verify eligibility and benefits or click the Group Limitations link to confirm which plan the member has.
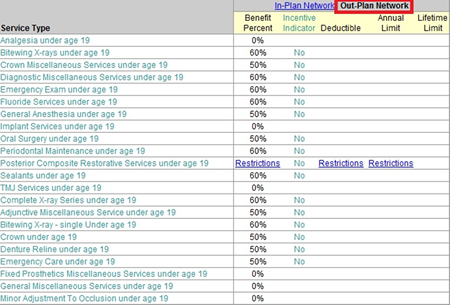
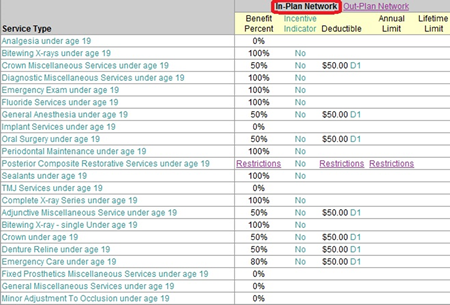
When checking eligibility and benefits, Benefit Tracker will default to the out-plan network. If you do not participate as a preferred (PPO) provider, these benefits apply when the member is seeking services at your office. Please note not all services are included on this screenshot. For additional benefit information, log into your Benefit Tracker account.
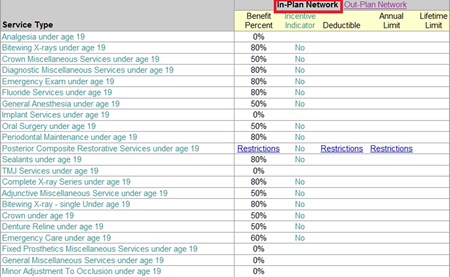
If you are a preferred (PPO) provider with ODS, click on the in-plan network benefits. Pediatric benefits will display at the top as shown below. Log into Benefit Tracker for a full list of in-network benefits.
Exclusive Provider Option (EPO)
The EPO plan utilizes the select group of dentists that have contracted with us at the preferred rate (PPO). The difference between the EPO plan and the PPO plan is that members must receive treatment from a contracted PPO dentist to receive any plan benefits. If a member on the EPO plan seeks treatment from a non-PPO dentist, ODS will not pay any benefits and the dentist can bill the member the billed charge for their services. However, if you are not a PPO dentist, it is important you let EPO members know this information up front so they aren't surprised later.
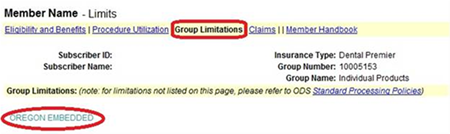
- To identify an EPO Plan on Benefit Tracker:
Insurance type will specify PPO (Dental Preferred), but Group Limitations will show EPO Family Plan.
Family plan is part of the plan name and doesn't mean the whole family is covered. - These plans can be purchased by individuals/families, small groups and large groups so group numbers and group names may vary. Below is an example of an EPO family plan, benefit percentages will vary by plan.
- The EPO plans use the Delta Dental PPO network as the in-network plan, so you need to look at the benefit percentages for in and out of network to confirm which plan the member has. You will not be able to tell a plan is EPO simply by looking at the ID card or the Benefit Tracker Insurance type.
- The only benefit available for seeing an out-plan provider (Non-PPO) is for emergency services, see screenshot below, which can be found under Group Limitations.
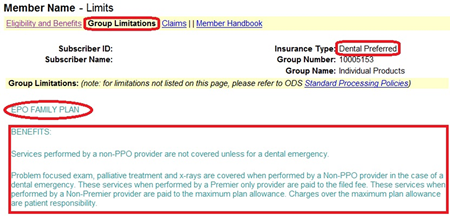
When checking eligibility and benefits, Benefit Tracker will default to the out-plan network. If you do not participate as a preferred (PPO) provider, these benefits apply when the member is seeking services at your office. Please note not all services are included on this screenshot. For additional benefit information, log into your Benefit Tracker account.
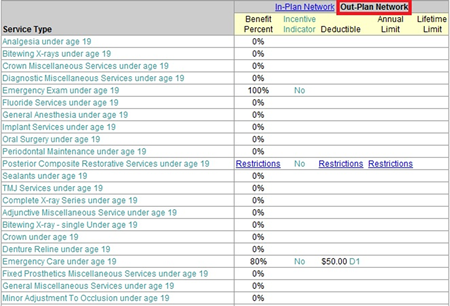
If you are a preferred (PPO) provider with ODS, click on the in-plan network benefits. Pediatric benefits will display at the top as shown below. Log into Benefit Tracker for a full list of in-network benefits.
Embedded Pediatric Dental
Another option for obtaining pediatric dental services is through a new plan offering which is part of the Affordable Care Act – medical plan with embedded pediatric dental benefits. This plan utilizes the Premier network and the deductible and out-of-pocket maximums are comingled.
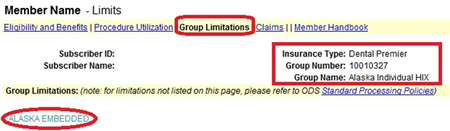
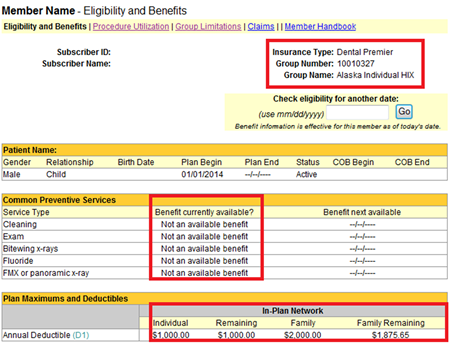
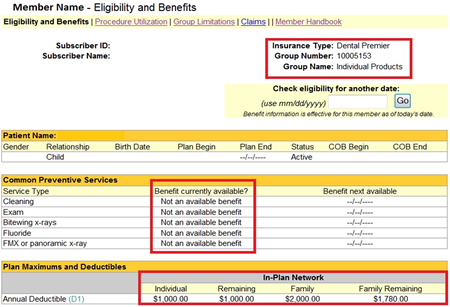
- To identify an embedded Plan on Benefit Tracker:
Large deductible listed under Plan Maximums and Deductibles (since the medical and dental deductible is shared)
If the deductible has not been met, common preventive services will be listed as "not an available benefit." - The Group Limitations link will also identify the plan as Oregon Embedded.
Medicaid
The Medicaid Plan (formerly Oregon Health Plan) utilizes a select group of dentists who provide services at a contracted rate. ODS administers this plan for the State of Oregon as well as several Coordinated Care Organizations. Providers have the option of limiting the number of new Medicaid patients they see in a month.
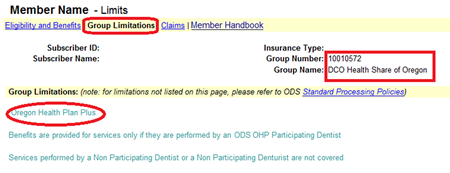
- To identify a Medicaid Plan on Benefit Tracker:
The Group Name and Group Number will be specific to the CCO the member is assigned to.
The Group Limitations link will also identify the plan as an Oregon Health Plan.
Additional Plan Notes
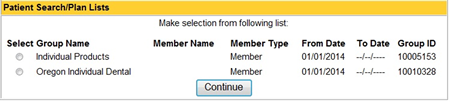
ACA requirements include pediatric services as an essential health benefit. Because of this, some children may have multiple plans. For example, they may have an embedded dental plan along with a stand-alone dental plan. This makes it even more important to check patient benefits on Benefit Tracker. This application is programmed to alert you with a pop up box when a member is double covered with any of our dental plans.
We're sorry, we don't currently offer dental plans in Washington. Use the dropdown at the top of the page to view dental plans in Oregon or Alaska.
With the healthcare exchange now in full swing, you may be wondering how it will affect you and your dental office. We’re here to help answer some of the most frequently asked questions by dentists.
What is the Affordable Care Act?
The Affordable Care Act (ACA), also known as the Patient Protection and Affordable Care Act, was passed into law on March 23, 2010. The ACA has many components to it, one of which is the marketplace exchanges where consumers may shop for their healthcare plans. The marketplace exchanges opened for business October 1, 2013, selling plans with effective dates in 2014.
For more information on the marketplace exchange in Alaska, please visit the federal website at www.healthcare.gov.
What are essential pediatric benefits?
ACA also has essential health benefit requirements which include essential pediatric benefits. Starting January 2014, most individual and small group insurance plans will have pediatric dental benefits. This coverage may be through a pediatric only plan and/or through a more traditional dental plan which covers the whole family. Large plans could also have this pediatric dental benefit in some cases.
The result of the essential pediatric benefits is that families may have children under 19 with different benefits than the adults or situations where only the children have benefits. It could even happen that the adults and children have different insurance carriers.
From a plan design standpoint, essential pediatric benefits require that preventive care is covered with no out of pocket for in network services and that essential services are covered without an annual limit for in network services. In addition, there are certain benchmark standards for essential pediatric benefits which could result in differences in benefit between adults and children.
In some cases, dental may be offered through a dental plan “embedded” in a medical plan. Embedded means there is only one policy which includes medical and dental coverage. Because there is one policy, the deductible is shared as well as the out of pocket maximum. We will be offering a plans with embedded dental, but you will still send in your claims with the same process as you would for any other dental coverage through Delta Dental of Alaska.
What plans will Delta Dental of Alaska offer?
We are selling individual and group policies both through the new marketplace exchange and direct like we do currently. Consumers eligible for a tax credit/subsidy must purchase through the marketplace exchange to get their credits.
What does this all mean to me, the dental office?
This means that beginning January 1, 2014 your office may begin to see more of your non-insured patients now having health coverage. The good news is that there may be more children with dental benefits and, therefore, more potential business for many dentists especially those who treat children.
If you have any questions, please contact our Dental Professional Relations department toll-free at 888-374-8905.
Also, to learn more about the Affordable Care Act, please visit our Learning Center at www.modahealth.com/shop/learning-center.
Examples of Delta Dental of Alaska Plans as seen in Benefit Tracker
Premier Plans
Delta Dental Premier is the plan that allows patients to choose from the widest possible list of network dentists. The dentist is reimbursed at his/her accepted filed fee.
- To identify a Premier Plan on Benefit Tracker:
Insurance type will specify Dental Premier - Group Names and Group Numbers will vary depending on the Employer Group.
Embedded Pediatric Dental
Another option for obtaining pediatric dental services is through a new plan offering which is part of the Affordable Care Act – medical plan with embedded pediatric dental benefits. This plan utilizes the Premier network and the deductible and out-of-pocket maximums are comingled.
- To identify an embedded Plan on Benefit Tracker:
Large deductible listed under Plan Maximums and Deductibles (since the medical and dental deductible is shared) and Alaska Embedded will display under Group Limitations.
- If the deductible has not been met, common preventive services will be listed as “not an available benefit.”
Questions?
If you can't find an answer, please feel free to contact our Customer Service Customer Service Customer Service
Questions?
If you can't find an answer, please feel free to contact our Customer Service
Employer web tools
Benefit Tracker
Check benefits, eligibility, incentive and utilization
Producer web tools
- Fully Insured Quotes (1-50)
- Equal Funding Quotes (25-99)
- Corporate reports
- eCommissions






Hello.
We have exciting news to share. ODS is changing its name to Moda Health.
Moda comes from the latin term "modus" and means "a way". We picked it because that's what we are here to do: help our communities find a way to better health.
Together, we can be more, be better.
Please select the state you live in, or the state where your employer is headquartered, so we can tailor your experience:

Hello.
Please select the state you live in, or the state where your employer is headquartered, so we can tailor your experience:
Changing your location to Oregon
You can return to your previous location in the site header.